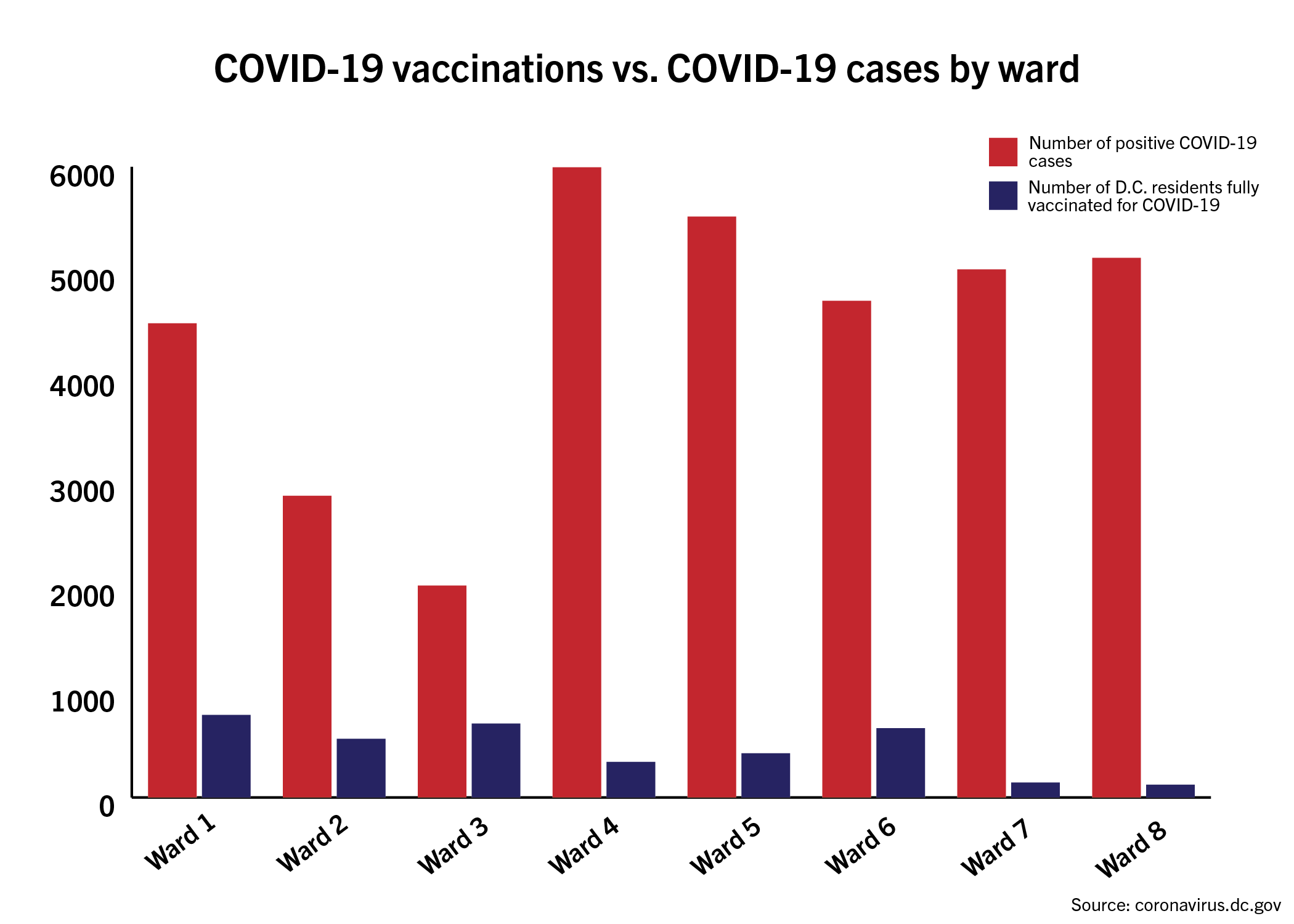
The area encompassing GW has logged one of the highest vaccination rates in the District while recording the second-lowest number of positive cases of any ward, according to city data last week.
The data reveal that the majority of initial vaccinations for residents aged 65 and older have been administered in the central areas of the city, where White residents make up a majority of the population. Experts in public health and epidemiology said the current model for vaccine distribution pits groups against each other instead of focusing on equitable distribution that addresses racial and ethnic disparities.
Sidney Lee | Graphics Editor
Arthur Reingold, a professor of epidemiology at University of California, Berkeley, said socioeconomics, education and housing make up social determinants of health, which can determine people’s access to public health resources.
“People on average of different racial and ethnic groups have different levels of income, education and housing,” he said. “These are all standard social determinants of health, some of which increase exposure to dangerous things, whether it is lead in water or air pollution or infectious agents. Some of it is less access to quality health care in a timely way.”
Residents 65 and older in Ward 2, where GW is located, have received more than 1,700 doses of the first round of vaccinations as of late last month while logging less than 2,800 positive cases as of Wednesday, according to the District’s website. Ward 3, tallying the lowest number of positive cases of any ward at less than 2,000, logged more than 3,600 shots of the first round of vaccinations for residents aged 65 and older as of late last month – the highest number of any ward – according to the website’s vaccination data.
The majority of COVID-19 cases have been concentrated in Wards 4, 5, 7 and 8, where Black residents make up at least half of the population, according to the District’s COVID-19 website.
Mayor Muriel Bowser has also proposed that city officials consider the use of a waitlist for vaccinations to lessen the chances of vaccines expiring while vaccinating more at-risk residents.
Ward 4, which has tallied 5,888 positive cases – the highest among all wards – has received 339 complete vaccinations as of last month, according to the website. Black residents make up almost half of Ward 4’s population while White residents make up less than a quarter.
Ward 8, logging the third-highest number of cases within the city at more than 5,000 cases, has received just more than 120 complete vaccinations, the lowest number of any ward, according to city data.
Black residents have accounted for three quarters of the city’s total COVID-19 deaths despite making up just less than half of the total population.
LaQuandra Nesbitt, the director of the D.C. Department of Health, said at a press conference that the allocation of vaccines to D.C. is “dismal.” She said the current supply prevents the District from implementing tiers that would prioritize certain populations, like elderly residents and health care workers, for the vaccine.
“Even with our best plans, and as rolling out the phases and the tiers two weeks ago, we are still in a position where we cannot implement fully any tier of a specific phase,” Nesbitt said at a press conference last week. “Our goal of creating tiers within our phases was that we would be able to fully implement a tier of a phase, but we can’t even manage to do that with the dismal amount of vaccines that we are receiving.”
Alison Reeves, a D.C. Health spokesperson, deferred comment to past press conferences where city officials have discussed vaccine distribution.
The D.C. Council urged Nesbitt in a conference call to prioritize geographic regions hit hardest by positive cases earlier this month. While the complete prioritization of vulnerable geographic regions was not agreed upon, Bowser announced Jan. 15 that D.C. Health would provide additional appointments in Wards 1, 4, 5, 7 and 8 to residents 65 and older or working in a health care setting.
An advisory committee – consisting of public health experts within the District, including some GW professors – has been working to advise D.C. officials on a plan of action for vaccine distribution.
Joshua Barocas, an assistant professor of medicine at Boston University, said creating tiers and conditions within already existing phases only exacerbates disparities in vaccine distribution because it places certain groups of people above others.
“Specific to vaccine rollout, part of what I think has happened is we’ve developed this, in our prioritization scheme, we have developed a sort of ‘Hunger Games scenario’ where everyone is fighting to get in line first,” Barocas said. “Everyone believes that they should or their group should be put in line ahead of somebody else, but in the whole discussion, instead of prioritizing the sub groups, which is what we’ve done, we’ve developed an elaborate scheme of subgrouping people.”
He said public health authorities and local officials should focus more on responsible allocation in light of the scarcity of vaccines available to residents within the city. He said the city’s phased rollout can create roadblocks in distributing expiring vaccines to at-risk populations that cannot obtain the vaccine in particular geographic regions.
“Many hospitals that have had vaccines allocated to them have vaccines sitting in their freezers simply because they can’t vaccinate outside of a certain subphase,” Barocas said.
Suma Vupputuri – an epidemiologist for the Mid-Atlantic Permanente Research Institute, an organization that researches health policy – said monitoring factors, like prior discrimination and trust in health care services, are essential in analyzing vaccination distribution for potential trends.
“We know that there are many well-known factors that affect racial disparities in health and health services utilization,” Vupputuri said. “I would be interested to know more about factors like prior discrimination and trust in health care providers, as it relates to racial differences in vaccine hesitancy.”