Researchers in the engineering school are using 3D printers to build artificial nerve tissues in hopes of treating patients with nerve and bone damage.
The team has been creating synthetic tissue made from biodegradable materials designed to temporarily support an injured or diseased organ as new tissue forms and published a study about their work last month. Researchers said they hope their cutting-edge use of 3D printing in medical research will help patients with tissue damage have faster recoveries.
Wei Zhu, a graduate student researcher in the School of Engineering and Applied Science, said the group of researchers in SEAS are looking to develop artificial substitutes to replace injured tissues in the human body. The team creates tissues with 3D printers on the third floor of the Science and Engineering Hall, using different varieties depending on the type of tissue that needs to be repaired.
He said researchers are developing artificial substitutes for bone, cartilage and neural tissue.
“We are pioneers actually in this field,” Zhu said. “And we actually try a lot of different 3D printing techniques and different tissue regeneration.”
Zhu said the team has tested many different types of materials to make the tissue, but they typically use a synthetic polymer, which is comparable to a plastic or rubber.
Researchers are examining the use of biodegradable materials, which would allow the tissue created in the lab to degrade in the body over time as the patient’s natural tissue healed.
“The goal is the scaffold will disappear in the human body with the formation of new tissue,” Zhu said. “The new tissue will be your own cells.”
He said the research could help patients with tissue damage caused by immune system diseases like lupus and rheumatoid arthritis.
“I believe my research is very interesting, and I believe someday that tissue engineering can save many, many people’s lives and improve many people’s life quality,” Zhu said. “I believe it will have a very, very broad application in certain areas.”
Zhu published a study April 12, along with Jonathan George, a doctoral student, Volker Sorger and Lijie Grace Zhang, both professors in SEAS. The study showed that the an artificial structure – created by 3D printers – will mimic healthy tissue in a damaged area as new cells multiply.
The team used red laser light to activate the neural stem cells on the 3D printed synthetic tissue, where a combination of artificial and natural tissues would promote cell growth.
Zhu said the project was a collaboration between Sorger’s lab and Zhang, who was Zhu’s professor. He said Sorger provided the lasers in his lab.
The researchers received funding from the University, the National Science Foundation, the U.S. Army and the National Institutes of Health.
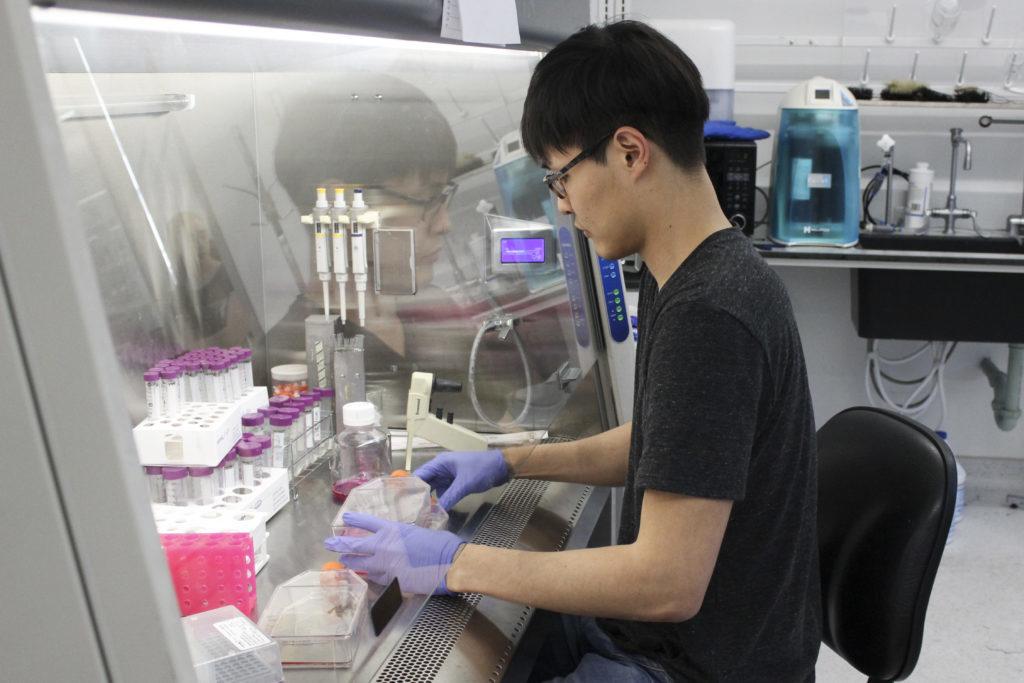
Se-jun Lee, a doctoral student focusing on materials science and tissue engineering, said he became interested in this type of research because he was looking for a way to combine engineering with biological and neurosciences.
Lee said when researchers create synthetic tissues for injured joints and softer damaged tissues, they craft malleable materials, typically made out of gelatin and collagen. For bones and cartilage, the material has to be rigid, he said.
Lee said the goal is to have the synthetic tissues interact with the native tissues in a way that does not cause inflammation for the patient.
“The one thing you have to think about is the mechanical properties of the scaffold,” Lee said. “You have to withhold all those mechanical strengths, the pressures, the walking, just standing, all those pressures you have to endure.”
Lee said this type of research involving 3D printing could eventually lead to more successful organ transplants. He said that complex organs, like livers and hearts, could be replicated by taking a 3D model and creating the organ using the patient’s own cells.
“That would be a really big breakthrough,” Lee said. “I’m not sure it’s going to happen in the near future, but a lot of studies are doing the research in those kinds of areas.”